These two words are quite similar in listening comprehension, so many people who pronounce the words "arthritis" and "osteoarthritis" do not even suspect that they are completely different diseases, although they are associated with joint problems. Both of these diseases, in fact, are very serious and it is worth knowing what the difference between arthritis and osteoarthritis is, if only to avoid putting yourself in an awkward position in a conversation, because the topic of health is one of the "eternal" topics when aperson communicates with another.
What is arthritis
Arthritis is a disease that affects most middle-aged people (under 40), although there may be exceptions. According to statistics, few people suffer from arthritis, no more than 2% of the total population. However, in essence, arthritis is a severe inflammatory process in which joint problems are only the visible part of the widespread inflammation.
In arthritis, the root cause of the disease is hidden much deeper than the swelling of the joints, as well as pain that does not leave the patient even during the night rest period (sometimes these pains only intensify). The cause of this inflammation can be an infection or a malfunction of the immune system. Joints aren't the only organs affected by inflammation. Often a powerful blow falls on such internal organs of a person as the liver, heart and kidneys. If the problem of arthritis is ignored, it is very dangerous not only for human health, but also for his life.
What is osteoarthritis
Osteoarthritis, in general, is an age-related change that a person undergoes, most often closer to the middle of the second half of life. Quite often, the mechanism of development of arthrosis is provoked by severe injuries in the form of fractures and damage to the joints in people over the age of 45.
Medical statistics say that osteoarthritis affects every third over 50 and every second over seventy. In general, about 10% of the inhabitants of our planet suffer from osteoarthritis. Most often, osteoarthritis affects the knees and hip joints in the elderly. In addition, the joints of the fingers and ankle can be prone to osteoarthritis.
The reasons for the development of diseases
It is clear that the causes of each of the diseases are completely different.
For arthritis, these can be:
- Injuries of various origins, to a greater extent, recurrent recurrent injuries associated with occupational activities can cause the disease;
- Infections such as tuberculosis, fungal infections, SARS, flu;
- Lack of vitamins and consequent imbalance of metabolism;
- Overloading of the body;
- Nervous system disorders;
- Malfunctions of one's own immune system;
- Having a genetic inherited tendency to arthritis.
Arthritis is frequent companions of people in professions such as seamstress, hairdresser, masseur, loader, construction worker.
Regarding osteoarthritis, the factors in the development of the disease are:
- Excess weight that affects the functioning of the joints;
- Bad nutrition;
- Prolonged hypothermia;
- Previously (perhaps even a long time ago) suffered various types of injuries;
- Intoxication of the body;
- Metabolic disorders;
- Past infectious diseases;
- Manifestations of autoimmune disorders;
- Perthes disease, which manifests itself in an impaired blood supply to the head of the femur;
- Thyroid disorders;
Hereditary tendency to develop arthrosis, transmitted at the genetic level.
Troublesome symptoms in arthritis
In arthritis, there is severe pain in the joints, especially when walking or other physical activities. The joint itself swells noticeably and the skin around the joint becomes warm to the touch. Also, the skin may turn red. The patient develops a feeling of weakness, it is very difficult for him to make movements with the affected arm or leg. It is especially difficult in the morning after a night's rest. When pressing on the joint, the patient feels severe pain. When performing movements, the joints affected by arthritis can severely creak. The patient may have an increased body temperature, and the patient himself may have chills at this time. In acute arthritis, all symptoms appear simultaneously and suddenly. With chronic arthritis, symptoms increase slowly and gradually.
Symptoms of osteoarthritis

In osteoarthritis, doctors distinguish four main symptoms of the disease:
- Pain in the joints.The pain is severe and acute. It begins when the movement begins and subsides with the transition to a state of rest. At night, a person has practically no pain, and having chosen a comfortable position, the patient can sleep peacefully. Pain sensations increase as the disease progresses. The pain is even worse in cold and rainy weather;
- Nibble on the joints.Due to the reduced freedom and softness of the bone rotation, a loud crunch is heard in the joint. Experts distinguish arthritic crunch from a kind of "dry" sound. The more the disease develops, the stronger the creaking of the joints. A feature of the crunch in osteoarthritis is that the crunch is almost always accompanied by pain;
- Restriction of the mobility of the joint itself.With osteoarthritis, the limb is immobilized in many cases. This is due to the fact that the growth of bone formations occurs and the joint space narrows, which first leads to a limitation of mobility and then to a complete immobilization of the joint;
- Deformation of the joints.As a rule, this symptom is characteristic of the last stages of the development of arthrosis, when osteophytes grow.
The difference between arthritis and osteoarthritis according to the clinical picture
It is quite clear that arthritis and osteoarthritis have different genesis as diseases. If arthritis is the result of a malfunction of the immune system or an infectious disease, osteoarthritis refers more to diseases resulting from the aging process of the body. Accordingly, based on this, the clinical picture of the manifestations of arthritis and arthrosis will also be different.
Arthritis of the fingers

So, with arthritis of the fingers, the patient has severe pain that does not subside during rest and at rest. Additionally, the skin around the affected joints turns red.
Arthritis can affect a different number of joints from one (monoarthritis) to several (polyarthritis). The joints are swollen. The reaction to the pressure of the joint can be acute pain.
As for the creaking in the joint, it may or may not be present.
Arthrosis of the fingers
Occurs more often in the elderly and osteoarthritis appears about 10 times more often in women than in the stronger sex. The main site of localization is the joints between the phalanges of the fingers.
Any movement of the fingers causes annoying pain to the patient. However, at rest, pain is practically absent. The joints are swollen and there may be redness of the skin around the affected joint. Osteoarthritis is always accompanied by a "dry" crunch of the joints.
The same picture is observed in cases of arthritis and arthrosis of the joints of the toes.
Treatment with chondreoprotectors
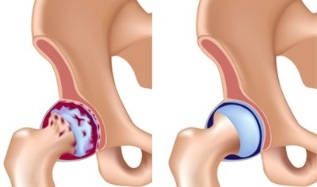
In arthritis and osteoarthritis, the cartilage is destroyed due to contact with the rough and rough surface of the bone. As a result, the synovial fluid production process is disrupted, the cartilage is deprived of nutrition, and the joint is deprived of the lubrication necessary for its normal functioning.
The chondroprotector prevents these pathological processes. The active ingredient of chondoprotectors is glucosamine and chondroitin sulfate. The dosage forms of the release of these substances are different and can be used by doctors depending on the situation.
Today, chondroprotectors are produced in the form:
- Solutions for injection;
- Tablets;
- Creams, ointments and gels.

Chondroprotective treatment must begin before the cartilage has completely collapsed. Unfortunately, such treatment is absolutely useless when the cartilage is destroyed. The next thing to remember when dealing with chondroprotectors is the duration of the course of treatment. The fact is that the cartilage restoration process is quite long, and the minimum course of treatment should be six months, but practice shows that treatment with chondroprotectors takes one and a half to two years on average. If the restoration is not fully completed, cartilage destruction resumes. As a rule, chondroprotectors do not have side effects on the patient's body, the maximum that is observed in practice is mild intestinal disorders. The only complication can occur when treating diabetic patients with chondroprotectors. During treatment, the insulin dose must be calculated correctly, as chondreoprotectors contain glucose. It is also not recommended to use the chondreoprotector during pregnancy, as well as for the treatment of children.
Today in the arsenal of doctors dealing with the treatment of arthritis and osteoarthritis problems, there is a number of effective drugs for treatment.
Treatment with chondroprotectors should be initiated under the supervision of a physician, otherwise the treatment may be ineffective.
Treatment with folk remedies
For arthritis, traditional medicine recommends several effective recipes:
- Apple cider vinegar.This substance is added to water (1 teaspoon for a glass of water). The resulting solution is drunk before meals;
- Potato wrap.Get some green tubers for the compress.
Washed, cut into pieces without peeling them. Potatoes are heated in water to a temperature of 38 degrees. Then a compress is applied to the sore spot. The potato layer should be 1. 5 - 2 centimeters. It is necessary to bet at night. The course of treatment in this way is from seven to ten days.
Ointments in the treatment of arthritis and arthrosis
In the early stages of the development of arthritis and osteoarthritis, the use of topical ointments can help in the treatment of the patient. A specialist will select the appropriate drug based on the examination results.


























